Medical Coding– What Is It And Where Are Its Issues?

2 min read
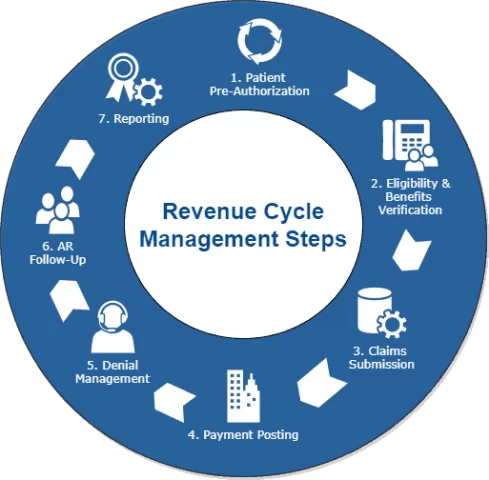
Reimbursement is a large part of how hospital systems generate revenue from payers (insurance companies), and is what we call ‘the backend’ of healthcare. Medical coding, though less visible to patients, helps physicians note and justify treatments and diagnosis for their patients; it is the backbone of how the healthcare system functions financially and contributes to strategies in revenue cycle management (RCM), a crucial component to hospital success that is equally on par to patient care and outcomes on the frontend. As healthcare policies evolve, RCM strategies and medical coding systems alter in parallel, and here we take a look at the basics of medical coding as well as a few key problem areas and white spaces.
1) What is medical coding?
a) RCM- Revenue cycle management; Steps include:
i) Documentation
ii) Patient details- demographics
iii) Eligibility of insurance claims check (pre-authorization)
iv) Filing of claims
b) Medical Coding Classifications:
i) ICD-11: newest classifications of diagnosis codes corresponding to diseases, abnormal findings, symptoms, etc, that are used for shorthand medical billing
ii) ICD-10-CM: clinical modifications of the previous version of coding system, namely, the ICD-10, and more used for outpatient applications due to more defined granularity of severity of disease and conditions.
iii) ICD-10-PCS: a more granular & detailed version of ICD-10, focused on procedures, equipment in inpatient settings.
iv) Current Procedural Terminology (CPT codes): procedural medical coding that is more surgically/medically focused with its primary purpose to standardize communication for administrative uses.
2) Problems in the area
a) Accuracy of coding- Lack of resources to record medical coding for each patient has become a larger problem, exposed by situations such as the COVID-19 pandemic causing medical overloads; Healthcare centers depend on staff levels to handle uptick in medical coding, and with providers and trained staff stretched thin at times, accuracy of coding is one of the first things to fall through, causing claim denial and lapses in administrative functions of hospital revenue cycles.
b) Bloated documentation (aka “Note Bloat”) – occurs when physicians notes include redundant information, either due to pressure of productivity/copy pasting information, uncertainty about coding requirements, or risk mitigation/defensive note-taking; these can cause a myriad of problems surrounding inefficient coding reviews, obfuscation of inaccurate medical findings, and lead to poor patient outcomes.
3) What can be done?
a) AI-ML leveraged error reduction- we are excited to see companies that take on aiding physicians in cleaning up patient notes or leveraging technology to ensure accuracy of assigning medical coding.
b) Automating RCM cycle- While companies such as Alaffia Health (disclosure: Tau portfolio) have tackled the preauthorization part of the pipeline, much needs to be done in the space of seamless coordination between payer enrollment and collections department of the cycle; we at Tau are also very much interested in full stack solutions of RCM for hospital systems.
Note from Amit Garg: Primary author for this article is Sharon Huang. Originally published on “Data Driven Investor,” am happy to syndicate on other platforms. I am a Cofounder and Managing Partner of Tau Ventures with 20 years in Silicon Valley across corporates, own startup, and VC funds. These are purposely short articles focused on practical insights (I call it gl;dr — good length; did read). Many of my writings are at https://www.linkedin.com/in/amgarg/detail/recent-activity/posts and I would be stoked if they get people interested enough in a topic to explore in further depth. If this article had useful insights for you comment away and/or give a like on the article and on the Tau Ventures’ LinkedIn page, with due thanks for supporting our work. All opinions expressed here are my own.






